Scarlet fever is a disease mostly affecting young children. The clinical manifestations are similar to measles, in the form of skin rashes. The disease is purported to be contagious and caused by a bacterium, as stated by a fact sheet from GOV.UK:
“Scarlet fever, is highly contagious and is spread by close contact with someone carrying the bacteria.”
The CDC states that the disease is allegedly spread by respiratory droplets and direct contact:
“Bacteria called group A Streptococcus (group A strep) cause scarlet fever. These bacteria are also the cause of strep throat. The bacteria sometimes make a toxin (poison), which causes a rash — the “scarlet” of scarlet fever.
Group A strep bacteria are very contagious. Generally, people spread the bacteria to others through
Respiratory droplets
Direct contact”
One of the first things about scarlet fever which makes one question the infectious narrative is the fact that the mortality of scarlet fever declined without the use of any vaccine.
The death rate had also plummeted way before the introduction of antibiotics.
Epidemiological data does cast a shadow of a doubt on the contagion dogma. In 1913 for example, Dr. Charles Chapin outlined that the incidence of scarlet fever was rare in families sharing the same houses as other families having cases of the disease.
In his reports, there were 4623 families with susceptible children, who were living together with other familes whose children were afflicted with scarlet fever.
Of these 4623 families, only 313 were simultaneously afflicted with the disease, which means that 93,23% escaped the disease.
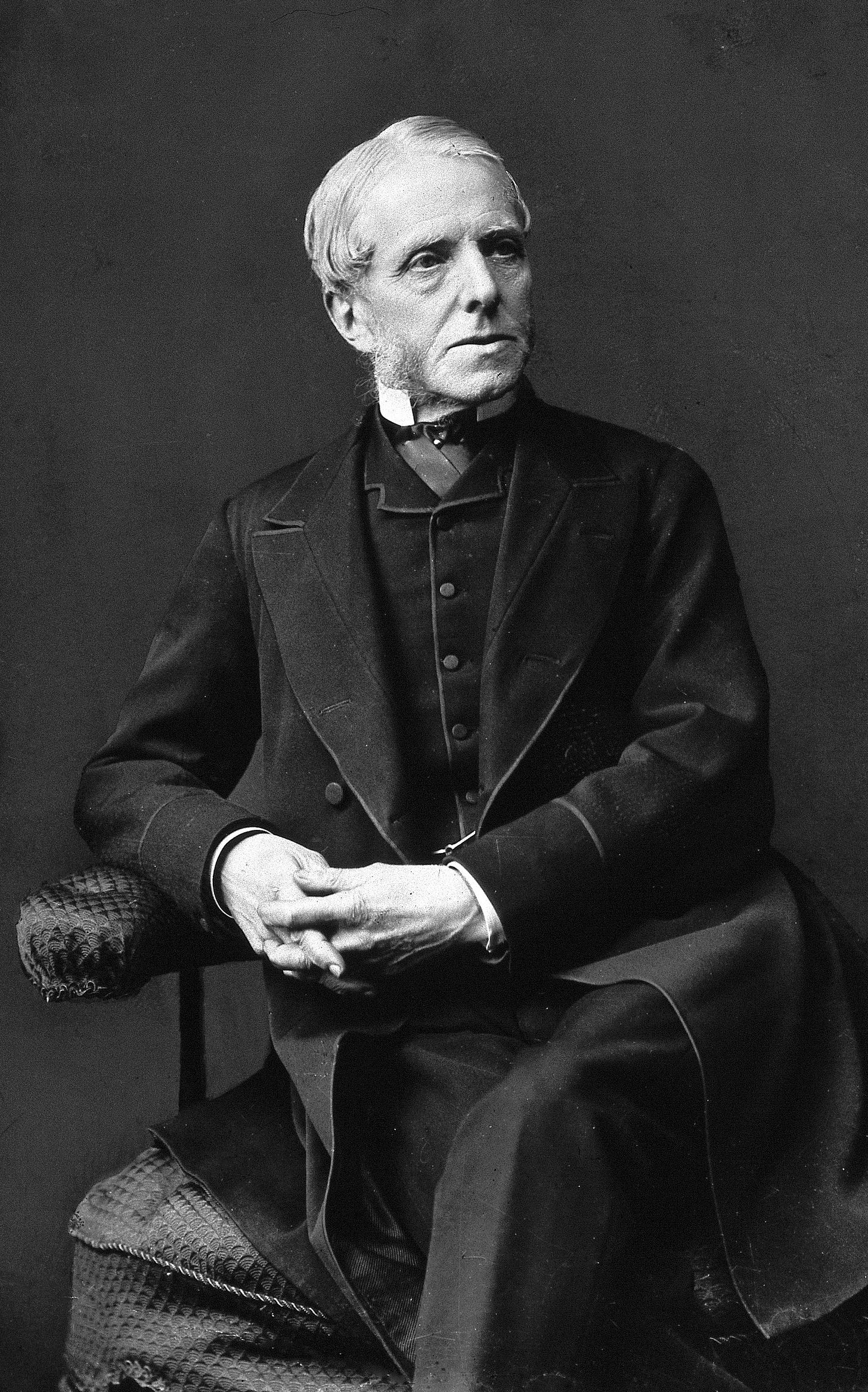
The non-contagiousness of scarlet fever is reinforced by Dr. Henry Littlejohn, who worked as a sanitary inspector. For 25 years he engaged in active sanitary work and had to deal with serious outbreaks of scarlet fever, and yet he never communicated the disease to his children or dependents. He did not know of any sanitary inspector who had contracted or communicated scarlet fever while in service:
“For twenty-five years I have been engaged in active sanitary work, and have had, with very limited staff, to cope with serious outbreaks of Cholera, Small-pox, Fever, Scarlatina [Scarlet Fever], Measles, and Hooping-cough, and although I have during that period brought up a large family, I have never communicated any of these diseases to my children or dependents, nor am I aware that any of the numerous sanitary inspectors who have acted under me have ever contracted or communicated these diseases while in the public service.”
Attempts to experimentally transmit scarlet fever to animals and humans did likewise not give any indication of contagion.
In their 1913 publication entitled Experiments on The Transmission of Scarlet Fever to the Lower Monkeys, G. Draper and J. M. Hanford make the significant remark that microbiologists working in the field were acknowledging that the attempts to induce scarlet fever in animals were unsuccessful. The animals did not develop scarlet fever when injected with alleged infectious material.
“The ordinary laboratory animals appear to be wholly refractory to inoculation with materials carrying the virus. There is general agreement regarding this point. The question turns upon the susceptibility to inoculation of monkeys, both higher and lower.”
They then examined the evidence for the inoculation of monkeys, but the results did not indicate any conclusive results.
“The symptoms upon which all the observers base their conclusions are varied and indefinite. All describe skin manifestations, but each differs markedly from the others.”
Draper and Hanford employed their own experiments in trying to induce scarlet fever in monkeys.
“The materials employed for inoculation were derived from patients in the early stages of scarlet fever.”
They inoculated several monkeys with the “infected” material but with negative results.
“After several experiments it became evident that the monkeys were highly resistant to infection by the microrganisms in the nasopharyngeal and ear secretions of human beings.”
Another series of monkeys were inoculated subcutaneously, submucously, and intraperitoneally, and again with negative results.
“This unsterile material was injected subcutaneously, submucously, and intraperitoneally without serious effect. Indeed, with the exception of sputum from a single individual, a general reaction was never observed, and in only two or three instances did local abscesses develop.”
A third experiment was performed with material composed of:
“(a) urine obtained under sterile precautions and found sterile by culture; (b) whole blood collected from a vein in paraffin-coated iced tubes, and injected, before clotting, intravenously into a monkey; (c) defibrinated blood; (d) sputum filtrates (Berkefeld); (e) filtrates of broth cultures of streptococcus from scarlatinous throats; (f) blood from scarlet fever cases mixed with ascitic broth and incubated at 37° C.
The researcher injected these brews into the monkeys in various places:
“The routes of introduction were through the mucous membranes, skin, stomach, joint cavities, blood stream, peritoneum, and brain.”
They even tried “repeated inoculations at three week intervals over a long period.”
But the results were negative:
“The animals stood the inoculation well and showed no reaction of any kind.”
Two series of experiments were subsequently undertaken. Series A. received subcutaneously the supernatant fluid from an emulsion of fresh tonsils from scarlet fever patients, whereas series B was given an emulsion made from tongue scrapings. Both series failed.
“Both series were negative.”
Draper and Hanford got desperate. In hopes of recieving a positive result in their experimental animals, they tried to employ even more brutal methods.
“The high degree of resistance shown by these animals led us to try two other modes of infection. The first was designed to overwhelm the animals with large, rapidly repeated inoculations of the infected material, and the second to employ methods which are known to lower the resistance of animals to infection.”
A poor monkey was injected with biological material obtained from scarlet fever patients. The monkey was injected in the brain, stomach, subcutaneously, and subsequently in the stomach again.
The throat, pharynx, and tongue were scarified and then swabbed with fresh throat swabbings of a five day old case of scarlet fever. The monkey was also injected one more time in the stomach.
After all of this torture, the animal showed no signs of illness or discomfort.
“Notwithstanding this amount of inoculation, the animal showed no rise of temperature above 40 ° C. and no signs of illness or discomfort.”
Draper and Hanford then drained a monkey of blood and another monkey were given an anaphylactic shock.
The drained monkey got injected with scarlet fever material and the throat was swabbed with alleged infectious material.
The anaphylactic monkey were injected with scarlet fever material into the brain two times, and one time in the guts. The throat was also swabbed with the material.
Once again, the results were negative.
“To diminish the resistance of the animals, the states of exsanguination and of anaphylactic shock were produced. In the first instance the animal was bled until severe symptoms of hemorrhage appeared and then a saline infusion was given. Following this, 50 c.c. of fresh whole blood were transferred directly from the vein of a twenty-four hour old case of scarlet fever into the circulation of the monkey. On the next day the monkey’s throat and pharynx were swabbed with material from the throat of the same case that had supplied the blood. No symptoms developed.
The last monkey treated was given a mild anaphylactic shock by injection of horse serum at proper intervals. On the day before the shock the animal received intracerebrally 2 c.c. of defibrinated blood from a forty-eight hour old case of scarlet fever. Four hours after the shock 3.5 e.e. of the same defibrinated blood were inoculated intracerebrally and 15 e.c. intraperitoneally. The pharynx was also swabbed with throat swabbings from the same case. No symptoms developed.”
The following year, a paper entitled Attempts to Produce Scarletina in Monkeys was published. The paper starts off by outlining a few studies with negative results.
“Landsteiner and Levaditi inoculated thirty-five monkeys of five different lower species with exudate from the throat and with the blood and lymph-nodes of scarlet-fever patients, by local application to the fauces of the animals and by intravenous, intraperitoneal and subcutaneous injections of scarlet-fever products without obtaining a seemingly positive result. Klimenko, making use of twenty monkeys of five lower species, was equally unsuccessful.
Shortly after the publication of Cantacuzene’s first papers, Dr. Park inoculated six monkeys with the blood of six fresh scarlet-fever cases, including several of the malignant type. The technic employed was the same as that described in Cantacuzene’s report. The results were completely negative.
Our few experiments are given herewith as an additional contribution to the proof that this class of monkey is immune to the virus of scarlet fever when inoculated by any method heretofore made use of.”
The researchers performed five experiments trying to induce scarlet fever in monkeys. They performed stomach inoculations and swabbed and sprayed the monkeys throats.
None of these experiments gave positive results.
“SUMMARY
The attempt to produce scarlet fever in monkeys and baboons by the faucial inoculation of streptococcus cultures or unfiltered exudates and discharges from scarlet-fever cases, as well as the intraperitoneal injections of filtrates of such exudates and discharges and of large quantities of blood, gave negative results.”
These results demonstrate that scarlet fever could not be transmitted to laboratory animals under experimental settings. This was acknowledged by various researchers.
What about human experiments?
In a 1914 human experiment, children with scarlet fever were put into wards with a total of 130 healthy children. They were allowed direct contact with each other. None of the children developed scarlet fever.
Dr. W. L. Scott, reported in a 1937 publication in The Lancet, the results of a careful investigation into the problem of “The Contact in Industry.” With regard to scarlet fever he found that, over a period of ten years, out of 17844 contacts with the disease, only 71 (0.39%) subsequently developed the disease.
In 1923, Dr. Ludvig Hektoen published a paper entitled The History of Experimental Scarlet Fever in Man. In the paper, Hektoen reviewed the human experiments attempting to transmit scarlet fever between sick people and healthy people. He concluded:
“This brief review of the recorded attempts to produce scarlet fever experimentally in man reveals that it is exceedingly doubtful whether a single positive case has been obtained. In view of the ease with which scarlet fever appears to be transmitted under natural conditions, the failure of the efforts at experimental transmission is a perplexing puzzle that awaits solution.”
Indeed, the attempts to transmit scarlet fever to healthy people were unsuccessful:
“The most recent attempts to produce scarlet fever in man experimentally are by Takahashi and by G. F. and G. H. Dick. Takahashi injected his five children, aged from 3 to 10, with the blood of a patient with scarlet fever on the sixth day. The blood was diluted in physiologic sodium chlorid solution with sodium citrate so that 1 c.c. contained 0.0001 c.c. of blood, and of this mixture four children received 1 c.c. subcutaneously and one, a 3-year-old boy, the youngest, 0.5 c.c. No symptoms whatever developed, and several weeks after his injection three of the children were injected with 0.15 c.c. and one, the youngest, with 0.06 c.c. of blood from a scarlet fever patient on the fifth day of a severe attack. In no case did any symptoms develop after the second inoculation. Furthermore, smearing the throats of two of the inoculated children with a mixture of the throat secretions and blood of a scarlet fever patient on the fourth day of the disease was also without any apparent effect. Takahashi is inclined to conclude that this experiment “proved the efficiency of the prophylactic inoculation against scarlet fever,” but in the absence of convincingly positive human control experiments the true significance of these experiments is not now determinable.
The largest series of inoculations to produce scarlet fever in man is that of the Dicks. Healthy men and women volunteers between the ages of 18 and 35, living in Chicago and without any history of scarlet fever, were inoculated in various ways; The blood serum of scarlet fever patients was swabbed on the tonsils and injected subcutaneously without any effect; whole citrated blood from scarlet fever patients was injected subcutaneously without effect; the filtered (Maasen or Berkefeld) throat secretion of early scarlet fever was swabbed over the tonsils and pharynx, used as a gargle and injected subcutaneously without effect; cultures of hemolytic streptococci from the throats of scarlet fever patients were smeared on the throats of thirty volunteers, seven of whom developed sore throat, leukocytosis and fever, but no rash, the others remaining perfectly well; finally, nine inoculations by means of throat swabs were made with the pure cultures of a pleomorphic bacterium obtained from the throat, blood and urine in the early stages of scarlet fever, and in two instances sore throat with fever, leukocytosis and a rash on the palate, but no cutaneous eruptions developed. The fact that no case of typical scarlet fever was produced in these extensive experiments naturally raises the question which the future may solve whether the results would have been different if the volunteers had come from rural communities.”

In 1924, G. F. Dick and G. H. Dick published a paper on scarlet fever. They stated that experiments on scarlet fever have long been hampered by failure:
“The intelligent prevention treatment of a disease must depend on a definite knowledge of its cause. Attempts to learn the etiology of scarlet fever have long been hampered by failure to obtain the disease experimentally.”
Animal experiments were unsuccessful because the symptoms produced were indefinite and inconstant:
“Symptoms that might represent scarlet fever in animals had been described by various authors; but these symptoms were indefinite and inconstant, and had followed inoculation with different materials and cultures. No organism had produced in animals a condition that could be accepted as experimental scarlet fever.”
The authors attempted to experimentally produce scarlet fever in various laboratory animals. But the results were unsuccesful.
“We attempted to produce experimental scarlet fever in guinea pigs, mice, rabbits, dogs, pigeons, and small white pigs. Monkeys were not used, because they had been so thoroughly tried by previous investigators that it seemed unnecessary to repeat their work. The animals were inoculated with blood from early cases, and with pure cultures of many different bacteria obtained from scarlet fever, also with ground-up organs from post mortems, and with mucus freshly obtained from the throat early in the disease. In this long series of animal inoculations, an occasional rash was obtained, and, less frequently, desquamation. But no one organism produced these symptoms constantly in any species; so the most essential evidence for the determination of the etiology of scarlet fever was still lacking.”
They concluded that animals were comparatively insusceptible to the disease, and human volunteers would be necessary for the production of experimental scarlet fever.
“We decided that animals are comparatively insusceptible to the disease, and that it would be necessary to use human volunteers for the production of experimental scarlet fever.”
They then performed experiments on young adults who had not been afflicted with scarlet fever before. The results were negative.
“Healthy young adults who said that they had not had scarlet fever were chosen. In the first series of human inoculations, reported in 1921, volunteers were inoculated with fresh whole blood and fresh blood serum from acute cases of scarlet fever; also with filtered throat mucus from early cases. The results of these inoculations were negative. Then since the hemolytic streptococcus is the organism most constantly associated with scarlet fever, and the one to which immune bodies are most constantly produced, the next volunteers were inoculated with pure cultures of hemolytic streptococci isolated from scarlet fever. In this series, we obtained an occasional sore throat and fever, but no rash.”












Great job Alhissla :)
The claim that scarlet fever was never demonstrated to be contagious is contradicted by well-documented scientific research conducted in the early 20th century by bacteriologists Gladys and George Dick. Through controlled experiments, the Dicks successfully induced scarlet fever in human volunteers by inoculating them with Streptococcus pyogenes—a bacterium isolated from a lesion on a nurse who had been caring for a scarlet fever patient. The development of scarlet fever symptoms following this inoculation provided strong evidence that the disease was transmissible.
Additionally, the Dicks' research identified the scarlet fever toxin by injecting sterile filtrates from S. pyogenes cultures into volunteers, producing the characteristic rash and "strawberry tongue" associated with the illness. The resulting "Dick test" allowed for the identification of individuals susceptible to scarlet fever, further confirming the toxin's role in disease development.
These findings align with the well-established understanding that scarlet fever is primarily transmitted via respiratory droplets from infected individuals. The research conducted by the Dicks, alongside subsequent studies, clearly demonstrates that scarlet fever is contagious and that its causative agent, S. pyogenes, can spread from person to person.
Dick GF, Dick GH. A skin test for susceptibility to scarlet fever. JAMA. 1924; 82:256–66